

Welcome to our new series, ‘Midwife Monthly’ where we share educational and informative content from trusted midwives for new parents from pregnancy, to birth and postpartum. This month, the amazing Beth Graham – founder of ‘This Is Your Baby’ , helping new parents with 7 of the most asked questions when it comes to feeding, sleep and development for newborns.
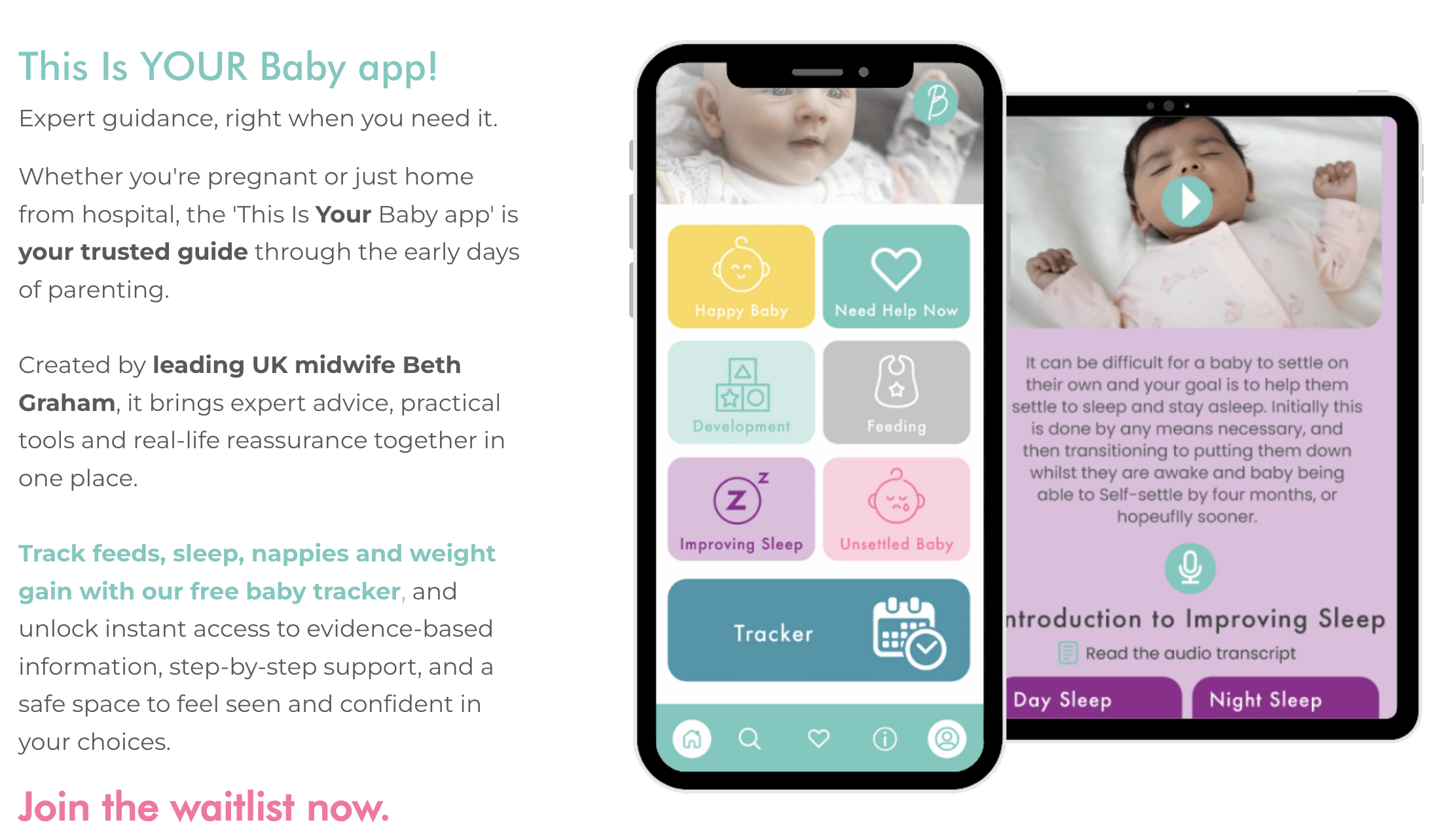
This Is Your Baby, is a new digital platform and soon-to-be-launched mobile app that brings clarity and confidence to new parents. It offers warm, down-to-earth advice on breastfeeding and bottle feeding, soothing unsettled babies, baby development, sleep, and emotional well-being – all grounded in Beth’s decades of practice-based experience.
Beth Graham is a practising midwife with over 35 years’ experience supporting families through every stage of pregnancy, birth and the first year. Over the course of her NHS and private career, she has supported thousands of parents with feeding, soothing, sleep, bonding and baby development – offering trusted guidance that’s rooted in what actually works for real families.
In the first days, weight is an important guide: babies should not lose more than 10% of their birth weight in the first five days and are usually back to birth weight by two weeks. After that, most gain around 30g per day, though anywhere between 15–60g is considered normal. Alongside weight, nappies are a very good indicator: by day five, most babies will have at least five wet nappies per day. Effective feeding also shows in your baby’s behaviour – you should hear or see swallowing, and your baby should settle and sleep between feeds rather than crying constantly, while also waking to feed rather than being too sleepy. Looking at the whole picture, rather than one measure alone, gives the best reassurance that your baby is feeding well.
Every baby is different and their needs vary from feed to feed. Breastfed babies regulate their own intake, and it’s normal for some feeds to be short “snacks” and others longer, fuller feeds. For formula-fed babies, a useful guide is 150–180ml per kg in 24 hours, divided into feeds, but this is only a guideline. Too much milk can cause discomfort and disturbed sleep, so it is important to pace feeds with pauses rather than encouraging continuous sucking. Watching for your baby’s cues – rooting, sucking, and then showing signs of being satisfied – is more reliable than focusing on fixed amounts. As your baby grows, you will learn what feels like a “minimum” and “maximum” feed for them, and this range will become more predictable over time.
“Sleeping through the night” is often defined as a five to six-hour stretch rather than a full 12 hours. Newborns have very small stomachs – drinking only a few millilitres on day one, increasing gradually over the first week – so they need to feed often, day and night. Over time, as their stomach capacity grows and feeding patterns become more established, most babies naturally begin to sleep for longer stretches. Daytime feeding also plays a role: if your baby is well-fed during the day, they may begin to extend their night-time sleep sooner. It’s important to remember that disrupted sleep is normal in the first months and, while routines and consistency can help, each baby reaches longer sleep stretches in their own time.
In the early weeks, feeding regularly during the day helps ensure babies get enough calories and this supports longer stretches of sleep at night. Waking your baby every three to four hours during the day is usually recommended. At night, once a baby is feeding effectively and gaining weight as expected, it is generally fine to let them wake on their own. Healthy babies will naturally begin to stretch out the time between night feeds as they grow. The key is balance: giving plenty of opportunities to feed through the day without overfeeding, and trusting your baby to rouse for feeds when they need them at night. If you are concerned about weight gain or feeding effectiveness, always check with your healthcare provider before allowing longer gaps between feeds.
Babies all develop at different rates, and milestones are only guidelines. For example, some babies laugh at 12 weeks while others are closer to 16 weeks. Some roll at 3 months while others do not until 7 months. First teeth can appear any time from birth to over a year. What matters is steady progress across areas of development: physical skills (such as head control, rolling, sitting, standing), social and emotional development (smiling, laughing, interacting), and cognitive development (attention, memory, problem-solving). The best support comes from everyday interaction – talking, singing, playing, and giving babies opportunities to practise new skills in safe ways. Try not to compare your baby to others, but do seek reassurance from your healthcare professional if you are worried.
The World Health Organisation and NHS recommend introducing solid foods at around six months. By this stage, most babies can sit with support, have better tongue control, and can coordinate swallowing safely. Starting earlier is not advised unless recommended by a healthcare professional, and a baby’s digestive system is not ready before 17 weeks. At first, solids are about learning – tasting different foods, experiencing new textures, and developing the skills of eating. Babies still get most of their nutrition from milk, and offering too much food too early can reduce their intake of vital nutrients from breast milk or formula. Between 6–12 months, solid food gradually increases in importance, and by one year, most babies are eating three meals and two snacks alongside reduced milk feeds.
Crying is part of normal development, and up to 3 hours a day can still be within the normal range. When it is longer, there may be an underlying cause. Colic is unexplained, prolonged crying, often peaking at around six weeks and usually resolving by 12–16 weeks. Teething can cause irritability, drooling, and a desire to chew, though symptoms vary widely. Wind is often relieved by winding techniques and ensuring a baby is not swallowing too much air while feeding. It can be difficult to tell these apart, but monitoring patterns and keeping a diary of crying can sometimes help identify a cause. If you remain concerned or your baby is difficult to settle, seek guidance from your healthcare provider.
For more information about This Is Your Baby, visit: https://www.thisisyourbaby.com/